

Discussion forum for Pharma Quality events, Regulatory Actions
Warning letters, 483s, Recalls, Import Alerts, Audit observations

Warning letters, 483s, Recalls, Import Alerts, Audit observations

Indoco Remedies’ Goa Plant (FEI 3005124189) received a warning letter from the FDA following critical observations during an audit in July 2024. The violations of Current Good Manufacturing Practice (CGMP) observed include lapses in microbiology laboratory control, sterile area validation, smoke studies in ISO 5 areas and aseptic facilities, complaint handling, and failure of the Quality unit in reviewing Empower Error Messages.
FDA investigators observed numerous non-viable dark particles in the plates and filters used for microbiological testing. Additionally, the in-house prepared media plates did not possess the smooth surface needed to ensure maximum contact of filters to facilitate the growth of microorganisms present. The analysts failed to ensure adequate filter contact on the plates, which could compromise the accuracy of analysis. Indoco responded that it conducted a retrospective review of microbiological testing data and found that lapses such as uneven surfaces on media plates and air bubbles and analysts failing to ensure contact of filter on media were rare. However, the FDA considered the responses inadequate as they relied on documentation of events that were not being recorded by analysts. The FDA suggested a comprehensive independent review of all laboratory practices and conditions that could impact the accuracy of microbiology testing data.
The FDA also observed that the airflow studies (smoke studies) performed in the ISO 5 area were deficient, and the airflow could not be visualized due to excess smoke. This was a repeat observation, and the FDA expressed concern that previous actions taken to prevent recurrence and the training given to personnel were inadequate. The FDA asked Indoco to reperform airflow visualization studies.
The auditors observed several deficiencies and unsuitable conditions in ISO 5 Grade A areas, equipment, facility and procedures to prevent microbial contamination of sterile products. Some of these were repeat observations; FDA had cited similar cGMP violations during an audit at the facility in February, 2023. The sensors in RABS located above open bottle / vial conveyors block first air and laminar airflow, there are no procedure for cleaning and disinfecting the sensors, rough surfaces in the top interior corners and frame of RABS, in Grade A line conduit on electrical wires do not extend to the end of wires, open gap at end of conduits making difficult to clean and disinfect and the conduits are not part of cleaning validation. Pens are used in aseptic filling areas for documentation but these are not cleaned, tracked or monitored. Auditors witnessed poor operator practices in aseptic areas. An operator in the filling line was observed to be repeatedly touching and resting the hands on a HMI next to the RABS and did not wipe his hands and arm after repeatedly touching the surface. Auditors observed that the environmental monitoring did not include garment washers and dryers used to wash gowns for classified areas, and the risk assessment did not address contamination hazards caused by these garment washers and driers
The warning letter also flagged inadequate investigation of repeat complaints of blockage of the dispensing tip, which was attributed to improper storage of the product by customers and the formation of a film. This explanation lacked scientific rationale. Additionally, repeat complaints of missing tips and empty vials were repeatedly determined to have no quality impact, even though this conflicted with the finished product quality attribute for fill volume.
It was also observed that the firm’s procedures governing chromatography analysis and review of audit trails were inadequate. Personnel were unaware of the requirement to review the Empower Message Centre data, and the firm did not review error messages and a high number of “User Abort” messages. The USFDA 483 also observed lapses in sample reconciliation, sample and test solution traceability. Original label of a sample was observed in trash and missing quantity of sample though analysis is not yet initiated and analysis worksheet was blank. In the trash bin HPLC vials with vague labels were also observed which could not be traced to test solutions.
In its responses to the FDA, Indoco had proposed specific remediation for these violations. However, the FDA concluded that repeat failures and observations demonstrate that executive management oversight is inadequate, the firm does not operate an effective quality system, and the quality unit (QU) lacked authority and/or has insufficiently implemented its responsibilities. The FDA emphasized the need for Indoco’s executive management to comprehensively assess the company’s global manufacturing operations to ensure that systems, processes, and products conform to FDA requirements.
Inadequate Corrective Actions and Response
The warning letter offers several lessons. Unreliable impact assessments not supported by data and ineffective Corrective and Preventive Actions (CAPAs) do not satisfy the FDA. Another key point is that training by itself is not a CAPA; it is only an additional awareness-building program. If errors and deviations are repeated despite repeated training, it indicates that the real root cause lies elsewhere, and the investigations are inadequate to identify it. This also leads to the conclusion that the overall training program is ineffective, leaving firms to handle now two issues: inadequate investigation and ineffective training procedures and programs.
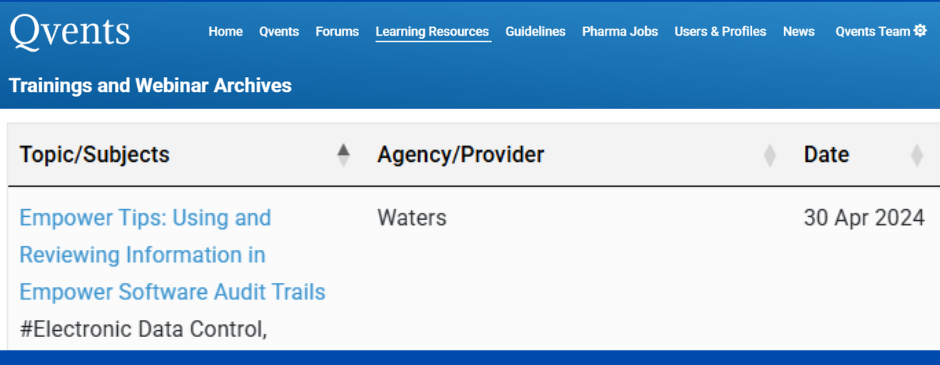
Access Waters Webinar on Empower Audit Trail @ Qvents Trainings & Archives
Leave a Comment
You must be logged in to post a comment.